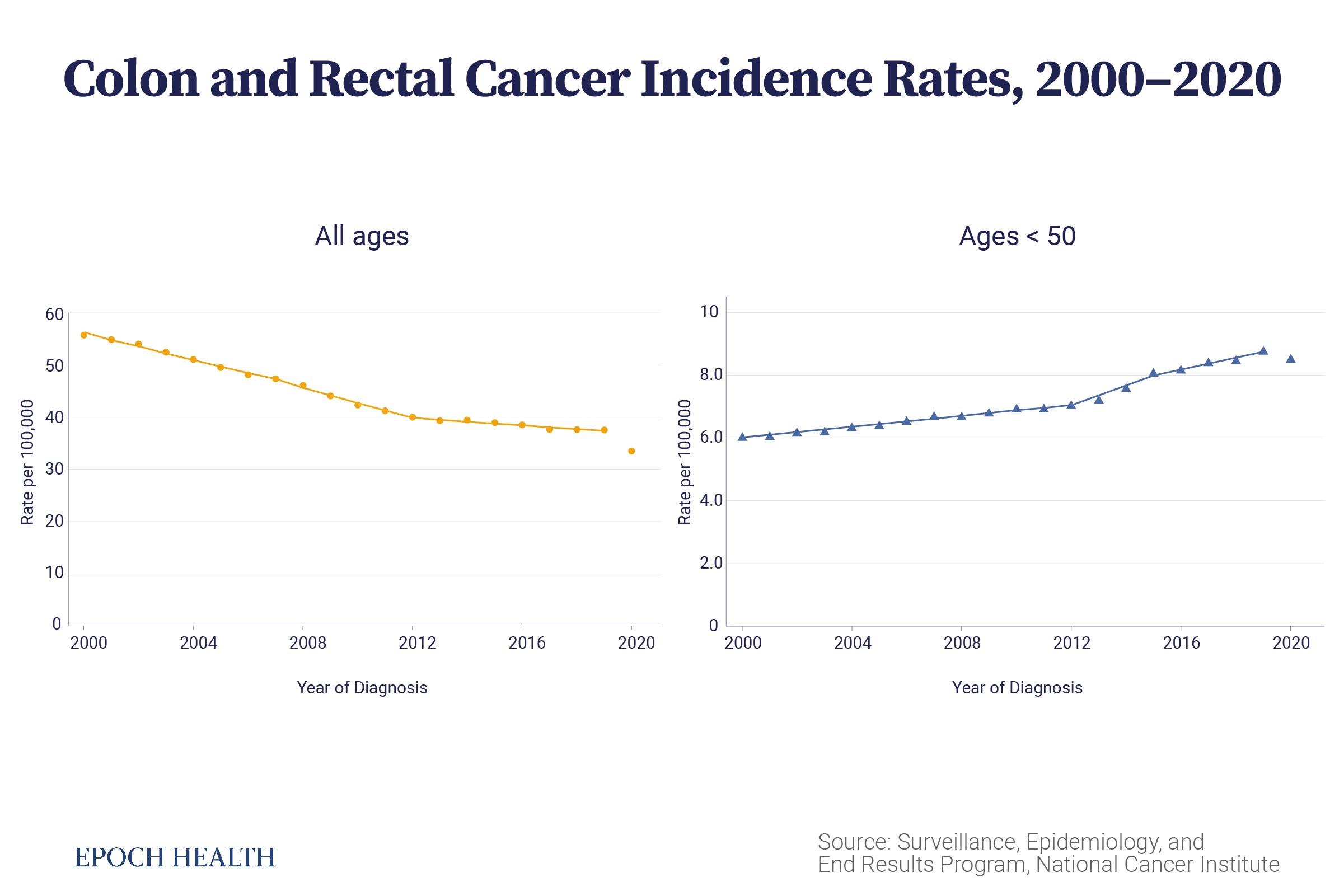
From 2000 to 2020, the incidence rate of colorectal cancer decreased by nearly half. However, among people younger than 50, the rate rose.
Overall, colorectal cancer incidence has been decreasing. But surprisingly, the incidence rate among young people is on the rise.
“Some new exposure” that emerged in the mid-20th century could be causing it, Rebecca Siegel, senior scientific director of surveillance research at the American Cancer Society, told The Epoch Times.
More Advanced Cancer
Abnormal cells in the gut lining can grow into polyps, and some polyps may become cancer after 10 to 15 years. Subsequently, they can metastasize to nearby lymph nodes or other parts of the body.

Dr. Kortmansky noted that upon microscopic examination, tumor cells in early-onset colorectal cancer patients “tend to have more aggressive histology,” a characteristic that seems to be somewhat related to the cancer being diagnosed at an advanced stage.
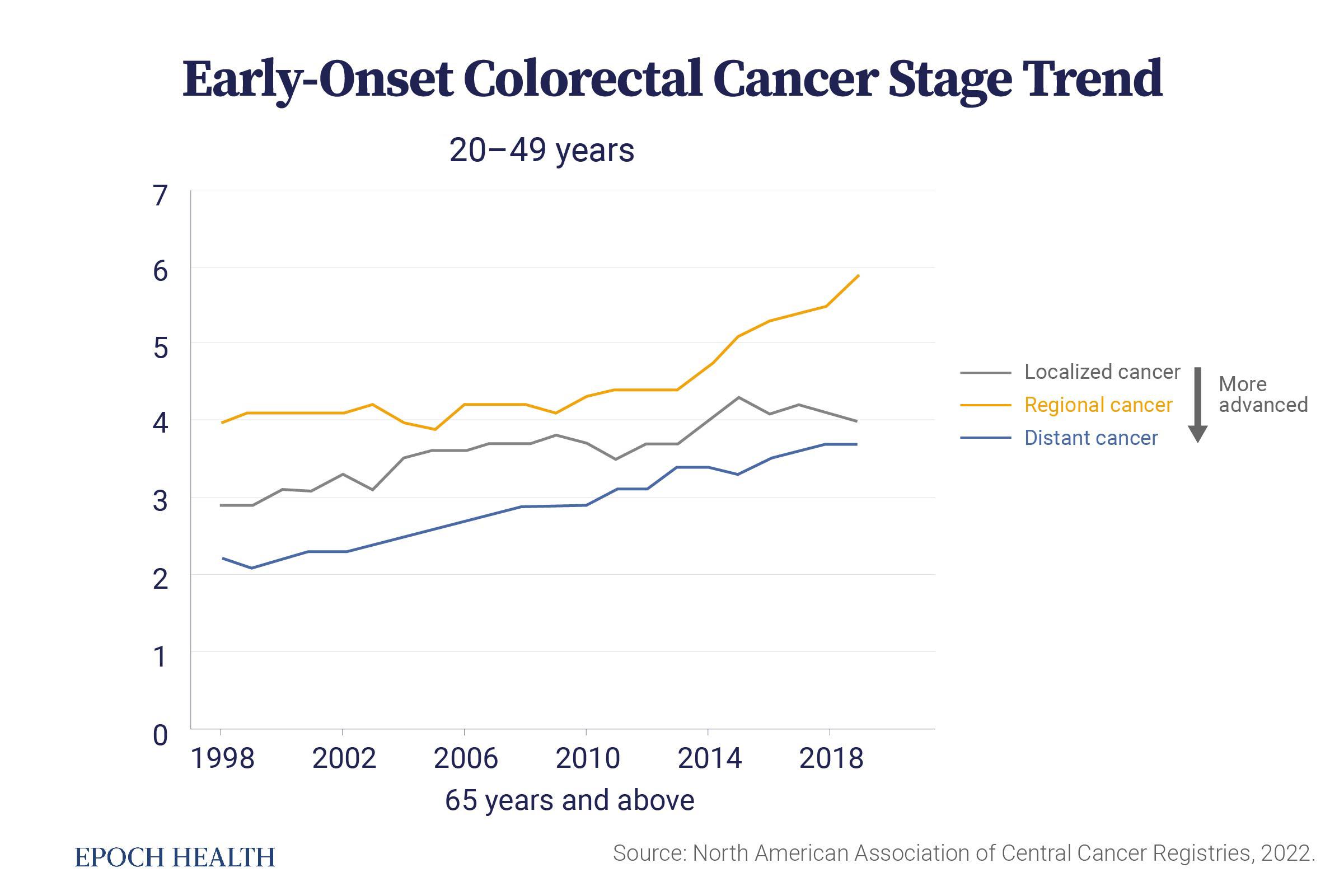
Many young people are misdiagnosed or have their symptoms overlooked.
“Doctors are not thinking about cancer in people in their 20s and 30s,” Ms. Siegel said.
By the time they are diagnosed, it is often in the late stages.
“But excess body weight accounts for only about 5 percent of all colorectal cancers,” Ms. Siegel said. “Probably it’s not obesity that is solely driving the increase.”
She cited African Americans as an example; despite experiencing the largest increase in body weight compared to other populations, they have seen the smallest increase in the rate of colorectal cancer incidence.
The Post-1950s Era
“While there are many known risk factors for colorectal cancer in general, these are based on older generations,” Ms. Siegel said, pointing out that there is a strong birth cohort effect in early-onset colorectal cancer among those born after the 1950s.
The more recent a person’s birth, the higher the risk, she said, noting that this indicates that “some new exposure is causing that higher cancer risk.”
Specifically, the incidence of late-onset colorectal cancer in the United States began to rise in the 1950s. In comparison, the incidence of early-onset colorectal cancer did not start to increase until the 1990s.
“There are so many changes in our lifestyle,” Ms. Siegel said. “Food supply’s very different; much more processed food. People’s lifestyle is much more sedentary.”
- Widespread use of antibiotics, especially in children
- Modernized dietary habits
- High consumption of added sugars, including sweetened beverages and high-fructose corn syrup
- The widespread use of food additives such as MSG, titanium dioxide, and synthetic food dyes
- Exposure to bright lights at night and changes in sleep patterns
Other experiences and exposures in early life during this period may also be associated with early-onset colorectal cancer, such as:
- Cesarean section
- Infant formula often replacing breast milk
- Increased maternal age at first and last childbirth
- Abdominal radiation therapy (especially early techniques that, due to precision issues, were more likely to damage normal tissues)
Sugary foods, such as high-fructose corn syrup, may be a primary culprit, Lewis Cantley, a professor at the Harvard Medical School Department of Cell Biology, told The Epoch Times in an email. He explained that the consumption of high-fructose corn syrup sharply increased in the 1960s and that over the next 20 years, the incidence of colorectal cancer rose in relatively young adults. These adults typically have KRAS mutations. The KRAS gene is an oncogene that can turn cells cancerous when mutated.
Carcinogenic Gut Microbiome
These new risk factors are silently changing our gut microbiomes.
“In recent years, people have only begun to realize the importance of the gut microbiome, but the evidence is still relatively preliminary. However, for gastrointestinal tract tumors like colorectal cancer, there is stronger evidence suggesting that certain bacteria species can indeed promote tumor formation,” Mingyang Song, associate professor of clinical epidemiology and nutrition at the Harvard T.H. Chan School of Public Health, told The Epoch Times.
Eight of the 14 types of early-onset cancers with increasing incidence are related to the digestive system, including colorectal, esophageal, extrahepatic bile duct, gallbladder, head and neck, liver, pancreatic, and stomach cancers.
 Not only do harmful bacteria contribute to carcinogenesis, but the loss of beneficial bacteria also affects their protective function.
Not only do harmful bacteria contribute to carcinogenesis, but the loss of beneficial bacteria also affects their protective function.“Our immunity is in the gut,” Dr. Sabine Hazan, founder and CEO of ProgenaBiome and a gastroenterologist, told The Epoch Times. “Everything you eat, you put on your skin, you breathe goes into your colon.”
Dr. Hazan explained that, like plumbers, doctors, lawyers, and other professionals with distinct specialized roles, each beneficial bacterium in the gut serves a specific function. The interconnections of these microbes doing something create immunity.
Bifidobacteria, in particular, are vital. It’s like “a marker of immunity,” she said. However, despite being one of the first bacteria to populate the infant gut and dominate in numbers, Bifidobacteria gradually decrease or even disappear as people age.
“Loss of Bifidobacteria definitely predisposes the young people to have, in my opinion, possibly colon cancer,” she said.
Unfortunately, once a particular strain of bacteria disappears, it is difficult to restore. Dr. Hazan explained that in most cases, orally ingested probiotics do not reach the gut but are killed by stomach acid. Some compounds in probiotics can kill Bifidobacteria.
“I like to think of loss of Bifidobacteria like a garden with no fruit trees. You destroyed a whole garden, and now, you are trying to regrow it. Unfortunately, if you have a storm, seeds you planted will not grow,” Dr. Hazan said. Therefore, preserving them from the start and preventing any potential factors that could kill them is best.

“If we have a toxic environment outside, then that typically translates to a toxic environment inside,” Dr. Nathan Goodyear, medical director of Arizona’s integrative cancer treatment center Brio-Medical and a board-certified physician, told The Epoch Times.
He explained that the gut microbiome is at the forefront of exposure to toxic substances, highlighting its significance.
‘A Legacy of Disease’
Nearly one-third of patients with early-onset colorectal cancers have a family history or genetic predisposition.
“The younger the patients are, the more likely they are to have a family history,” Dr. Kortmansky said.
However, there is another factor that is more important than genetics: epigenetics.
Epigenetic factors act on the surface of genes like keys to a treasure chest, either activating or silencing genes. For instance, when a cancer-suppressing gene is turned off, tumors can grow uncontrollably.
 Epigenetics can also affect our offspring, as they accumulate before a child is born. A mother’s diet, stress, and consumption of tobacco, alcohol, and drugs can all mark fetal DNA. Similarly, the father’s lifestyle and diet influence the epigenetic information in his sperm.
Epigenetics can also affect our offspring, as they accumulate before a child is born. A mother’s diet, stress, and consumption of tobacco, alcohol, and drugs can all mark fetal DNA. Similarly, the father’s lifestyle and diet influence the epigenetic information in his sperm.“We’re going to leave a legacy of disease for our kids, our grandkids, and our great-grandkids,” Dr. Goodyear said.
Different Screenings
“Colorectal cancer screening is one of only two cancer screening tests that can actually prevent disease,” Ms. Siegel said, noting that removing polyps can prevent cancer.
Ms. Siegel noted that among early-onset colorectal cancer patients, about 44 percent fall between the ages of 45 and 49. Increasing screening rates could help reduce the burden of the disease. She also mentioned that people with a family history of colorectal cancer or adenomas should begin screening earlier, depending on when the relative was diagnosed. For example, if a person’s sister or brother had an adenoma at age 45, they should probably start screening at age 35, but it’s important to discuss this with doctors.
It is worth noting that despite the rising incidence, the absolute risk of young people developing this disease is still very low. Therefore, Ms. Siegel suggests that those without a family history or prior polyp diagnosis can start with stool tests, which are convenient, cost-effective, and have minimal side effects.


Stool tests can be conducted annually, and those with positive results should undergo colonoscopy as soon as possible. If the colonoscopy reveals a bowel that “looks perfectly clear,” screening can be done every five to 10 years.
The Right Fuel
All things considered, “lifestyle may be the most modifiable factor” in preventing colorectal cancer, according to Dr. Kortmansky.
“If lifestyle is contributing to the acceleration of this process (early-onset colorectal cancer), then in turn, lifestyle is the means to reverse that trend,” Dr. Goodyear said.
He explained that we were not born to eat processed foods; most people’s gut health issues stem from not eating real food. First, we must return to a traditional and healthy way of life, eating real, natural, chemical-free, and additive-free food.
Consuming processed foods is like putting diesel in a gasoline car—an analogy Dr. Goodyear strongly agrees with. On the other hand, while research increasingly supports the benefits of probiotics, he stressed that natural foods, including vegetables and fermented foods, also serve as probiotics and prebiotics.
Dietary Fiber
Dietary fiber helps shorten the time that feces spend in the gut, reducing the contact between the colon wall and carcinogens. It also serves as food for probiotics, breaking down into short-chain fatty acids with anti-inflammatory and anti-cancer effects. A diet rich in fiber can help suppress harmful bacteria.
Calcium
Calcium can combat colorectal tumors in multiple ways. It helps reduce the carcinogenic effect of toxins on the colon mucosa. Calcium inhibits abnormal cell proliferation. A meta-analysis found that daily supplementation with 1,200 to 2,000 milligrams of calcium for three to five years reduced the recurrence rate of colorectal adenomas by 12 percent.
Vitamin D
Vitamin D can enhance the gut’s immune function. Many studies support vitamin D’s anti-cancer effects. A meta-analysis based on five studies found that people with a serum vitamin D level of less than or equal to 30 nanomoles per liter (nmol/L), or 12 nanograms per milliliter (ng/mL), had a 50 percent higher risk of developing colorectal cancer than those with a concentration of 82.5 nmol/L (33 ng/mL) or higher.
Vitamin C
Clinical studies have shown that vitamin C significantly increases microbial diversity and short-chain fatty acids in feces. A small-scale human trial conducted by Dr. Hazan demonstrated that vitamin C supplementation can enhance the abundance of bacteria from the genus Bifidobacterium.